People living with HIV no longer forced to lie to access treatment
AUSTRALIANS living with HIV will no longer be forced to lie about their symptoms to access early treatment following changes to the Pharmaceutical Benefits Scheme in effect as of today.
Prior to the changes, doctors were unable to prescribe HIV treatment to HIV-positive people without clinical symptoms and with CD4 counts above 500 — a clinical measure of the virus’ impact on a person’s immune system.
This arrangement required some people living with HIV to lie about symptoms in order to gain access to treatment if their CD4 count was not below 500.
HIV advocacy and medical organisations campaigned for the PBS restrictions to be lifted, and have welcomed the changes both for people living with HIV and for strategies to reduce HIV transmissions.
The restriction was originally in place before a range of new medications developed over the past decade or so made early treatment far more beneficial. Its removals now brings Australia into line with many other countries, including the US.
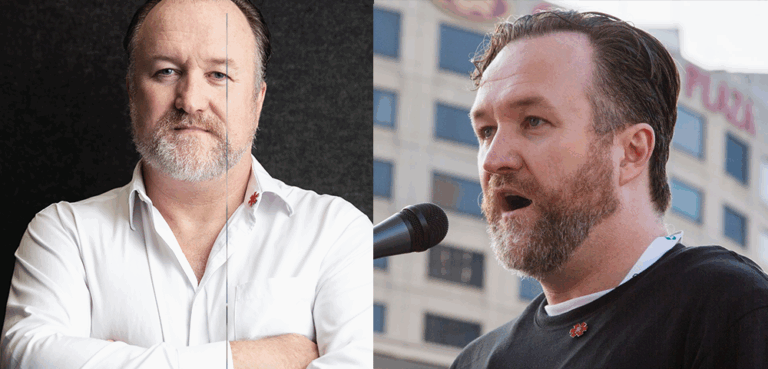
National Association of People with HIV Australia (NAPWHA) spokesperson Bill Whittaker told the Star Observer the restriction had put people living with HIV, as well as their doctors, in a difficult position. He said doctors were forced to find “generic” symptoms in order to meet the PBS requirements.
“Let’s say doctors and patients have had to take a generous view of the regulations — they’ve had to bend the rules. That’s been the case for a long time. I think that’s a really invidious position to put doctors and patients in,” Whittaker said.
He also argued the restriction was at odds with acknowledged best-practise approaches to HIV treatment.
“It just sends a confusing message. On the one had we’ve got leading clinicians and doctors and our own treatment guidelines saying treat early, yet on the other we’ve had this regulatory restriction that’s not allowed all people with HIV that choice,” he said.
NAPWHA has launched a public awareness campaign promoting the change, emphasising the health benefits of HIV treatment and its role in reducing HIV transmissions. The organisation also argued treatment can also help relieve the guilt, blame and anxiety of HIV-positive people afraid of possibly infecting others.
A study released last month found HIV-positive people on effective treatment and with a low viral load have an extremely low chance of passing the virus on to a HIV-negative partner, even during unprotected anal sex. Early and effective treatment is receiving increased attention in the community as a strategy for reducing rates of HIV infection, known as “treatment as prevention”.
Victorian AIDS Council/Gay Men’s Health Centre chief executive Simon Ruth welcomed the change and said the PBS change removed a barrier to implementing treatment as prevention. He echoed Whittaker’s position that the change was significant in allowing people living with HIV to choose whether or not to start early treatment.
“Of course this decision needs to be seen within the context of individual rights over their treatment and care. It needs to remembered that treatment decisions are really up to the individual, and whether they are willing and able to commence and adhere to treatment,” Ruth told the Star Observer.