
Victorian CHO Brett Sutton On Public Health Orders, HIV Care And LGBT Community
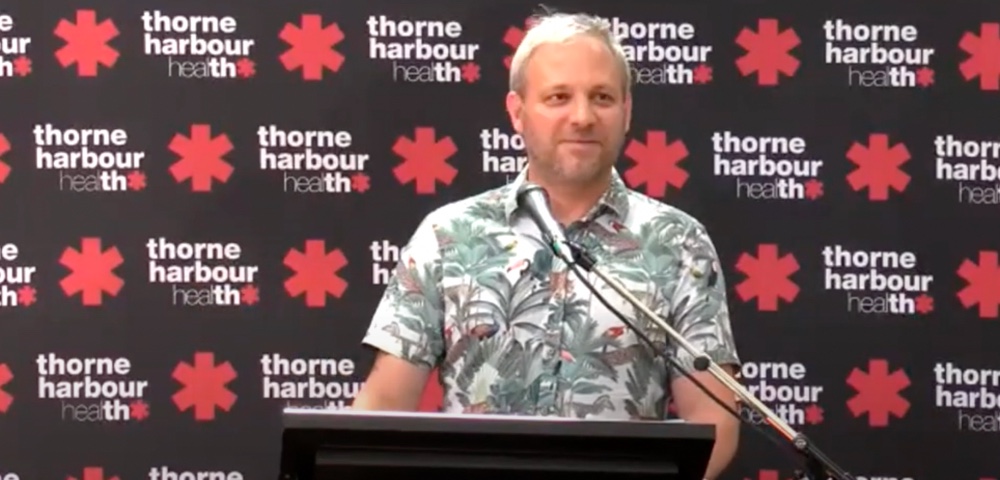
Victoria’s Chief Health Officer Professor Brett Sutton last week delivered the 30th Annual Keith Harbour Address at the 2022 Thorne Harbour Health Awards.
The Thorne Harbour Health Awards recognise “the outstanding contribution of individuals who have made a significant impact on improving the health and well-being of LGBTIQ+ communities and people living with HIV.”
This year the recipients included HIV clinician and researcher Professor Jenny Hoy (President’s Award), peer facilitator and outreach volunteer Tegan West (Greig Friday Young Leader Award) and Danny Gallant and Russell Oke (Life Memberships).
Special Service Award recipients included historian and principal assessor at Heritage Victoria Dr Marina Larsson, trans and gender diverse community advocate Starlady, volunteer, Derryn Pert, First Nations trans, non-binary teacher and activist Ricki Spencer and former Director of Rainbow Health, Marina Carman.
An Ordinary Guy Thrown Into Extraordinary Circumstances
Professor Sutton in his address spoke about the need to have uncomfortable decisions when dealing with public health.
“I’m an ordinary guy who has been thrown into extraordinary circumstances through the COVID pandemic of the last three years… I’ve sat in discomfort a great deal over the last three years – sometimes some extraordinarily uncomfortable situations,” said Sutton.
“These are not unique to COVID. There have been hugely controversial and contested spaces – especially for marginalised populations, especially for those who have had to struggle for their voice to be heard and for their rights to be exercised.”
Professor Sutton Spoke about his early clinical experiences at Fairfield Hospital in 1993 during the early days of the HIV and AIDS epidemic.
“One of my very first patients was a young HIV-positive man,” recalled Sutton. The man had been admitted to the ward on a public health order.
“He was dying, he had just days to live. It was my job to take blood on the ward every morning. I would go into his room every day to take his blood and I remember the security guards who would sit by his bed because he was under 24. hour guard. Now the guy couldn’t get out of bed, he couldn’t walk and he literally had days to live. But again, the framing of HIV in that context was that he had a 24/7 guard by his bedside to make sure that the community was kept safe.”
A Haven For Gay And Bisexual Men
Sutton said it was also one of his earliest experiences with palliative care. “It was very unusual again in as much as there was a man in his early 30s who wanted to talk through with his clinicians how he could stop taking his medication, how he could allow himself to die.”
“I’d been involved in palliative care before but I’d never been involved with someone who was such an advocate for himself, and where his clinicians were advocating so strongly for his own well-being at a time when he was dying. That had a profound effect on me because it was a strong voice in the last days of a man’s life about the exercise of his own agency.”
Sutton credited the now-closed Fairfield hospital for being a “haven, especially for gay and bisexual men”.
“They felt at home there. There were double beds in the wards for partners to stay over. It felt like the people who were looking after them, understood them and understood their priorities in life and in dying.”
“I think mainstreaming has been an important evolution in HIV care. Clearly, it’s important that people with HIV can be looked after by their GPs and community health centres across the state. You don’t have to find this one specialist expert tertiary hospital to provide care, but I think we need to try and keep the essence of what Fairfield was able to provide at that time, and what other services were able to provide, which is having that patient-centred, that community-centred view in everything that they do, and that’s what Fairfield did so magnificently.”
Uncomfortable Conversations
“There were lots of uncomfortable conversations at the Fairfield and I’m glad that I was part of them because it was a real part of my clinical development, a deeper understanding of the world, especially for HIV-positive gay and bisexual men in the 90s in Australia”.
Sutton spoke about the different approaches to the HIV/AIDS epidemic in the US and in Australia, the impact of which is felt even today in how it played out in these countries. The Victorian CHO said that some issues continue to be resolved like HIV notifications and criminal prosecution of people with HIV.
“There are issues of HIV and criminal justice that are still to be resolved,” said Sutton, clarifying that he was speaking in his personal capacity and not as a department policymaker.
“Let us all sit in uncomfortable conversations together, but bring our passion, bring our advocacy, bring our open-mindedness. If we go in with a compassionate heart and a genuine willingness to hear and a genuine willingness to change, then the policy that will play out over time will work in all of our stead for all of the issues that are near and dear to us,” Sutton said.









