The silver lining to an ongoing struggle
Last Sunday a group of people gathered in Fawkner Park, South Yarra, to remember the achievements of the Victorian AIDS Council/Gay Men’s Health Centre (VAC/GMHC) and it’s 25-year history promoting HIV awareness and prevention and assisting people living with HIV.
Among the picnic-goers was the VAC/GMHC’s first president, Phil Carswell, a key player in the state’s HIV prevention story from the outset.
-œ[The early -˜80s] was a horrifying time, mainly because you had this sense of great rolling inevitability -” this thing was coming, we didn’t know how big it was, we didn’t know who had it and who didn’t and we didn’t know how to stop people getting it in the first place, Carswell told Southern Star.
-œWe didn’t know where [the VAC/GMHC] was going to be in six months time, let alone 25 years time. That’s why it’s a remarkable achievement.
The VAC/GMHC began life as a humble meeting of gravely concerned people from Melbourne’s gay and lesbian community, stemming from a gripping fear of the mysterious new disease hitting the community.
Although 25 years marks the time since the first official public meeting in 1984, the seeds were planted in the years preceding.
Stories of the virus surfaced from abroad and in 1982 Sydney reported Australia’s first AIDS case, involving a US national.
As the shock waves hit, Australia was quick to mount a response to the great unknown.
In Victoria, by 1983, members of the newly formed ALSO Foundation had heard enough to know action needed to be taken and a medical subcommittee was formed.
-œWe’d heard the stories from Qantas stewards and leather boys with close links overseas who came back and told us people were getting sick and dying and no-one knew what it was and what was causing it, Carswell said.
Of the four key people involved in the subcommittee -” Ian Dunstan, Peter Knight, Chris Carter and Phil Carswell -” Carswell is the only one still alive, the others succumbing to HIV-related illnesses.
-œI remember going to bars and seeing people with lesions on their faces Carswell said. -œIt was like a tsunami, but a slow-moving one -” then once it hit, it didn’t stop. There were times when we were going to three or four funerals a month.
The first community meeting was held in June 1983 at the Royal Dental Hospital in Parkville. Community fear filled the auditorium. On stage, seven (mostly gay) doctors and an immunologist told the audience all they could about the disease.
-œThe mood in the room was very ominous -” -˜Oh my God, what’s happening here? What are we going to do?’ Carswell said.
He still has the notebook from that night with the advice given scrawled on the page: -˜Don’t fuck with Americans.’
-œWhen one of the doctors said that, people were looking at one another around the room because they realised they had in fact fucked Americans, Carswell said.
The Victorian AIDS Action Committee was established, with the responsibility to find as much information about the virus as possible.
Carswell said the early years saw him -œrunning around like a scalded cat recruiting volunteers, helping people get organised, acquiring information and answering frenzied media calls.
-œThe atmosphere was pretty paranoid. The gay community wasn’t really that strong or visible at that stage and the press were seeking dramatic headlines, he said.
-œWe were getting calls from the health department asking -˜What do you guys know about this?’, because they had no idea.
-œThere was panic everywhere -” childcare centres, schools, airlines, hospitals -” everywhere there was a human service involved. But they were more worried about dealing with gay men. They didn’t want to touch them, they didn’t want anything to do with them, Carswell said.
Carswell said the HIV epidemic changed the way public health policy is developed.
-œIt was the first time people with the infection actually took part in the policy development -” that’s never happened before, he said.
-œWe need to acknowledge that while it might have been as black as pitch and an awful time for everybody, and we lost a lot of really good people, the price we paid is that now our community’s grown up and accepted -” that we are a diverse community and we all have something to contribute.
Never has a health crisis been so political, and the HIV response in Australia is marked by those few who stood apart from the rhetoric and addressed the issues.
In November 1984, the Queensland Health Minister announced four babies had died from a blood transfusion using blood given by a gay man. A wave of AIDS hysteria and homophobia set off around the country.
Current VAC/GMHC executive director Mike Kennedy remembers this well, recalling the Queensland newspaper headline -˜Die You Bastard’.
-œThere weren’t HIV tests available at the time … so [then federal health minister] Neal Blewett realised something needed to be done to stop this hysteria and the lynch mob mentality, Kennedy said.
Blewett responded by calling emergency meetings with the state health ministers, calling HIV/AIDS the most serious public health problem since Federation. As a result, government funding started to flow. The VAC/GMHC received its first cheque Â-” for $50,000 -” from the state health department in March 1985.
-œBlewett realised unless something was done and unless the three sectors of government, doctors and researchers and the community worked together we’d all go down together, Kennedy said.
The federal health department moved quickly to set up a scientific and community body that could give the government sound advice.
-œSuddenly there were gay men, sex workers and injecting drug users sitting around tables having input into what kind of government policies were needed to deal with HIV, Kennedy said.
-œIn Queensland -” at a time when sex between men was still illegal, sex work was still illegal and injecting drug use was still illegal -” the government could still see beyond that kind of moral and law and order agenda and say, what is a pragmatic public health response … that was a huge and, in retrospect, pretty brave step for some of those conservative politicians to take.
By the end of 1985, 173 cases of AIDS had been diagnosed in Australia; by 1990, 9,286 people had been diagnosed and of those, 1,571 people had died.
When the safe-sex message hit and HIV rates began to tumble in Victoria in the mid-90s, the health promotion priority became lost and state funding resources began to wane.
In 1996 the VAC/GMHC restructured in a bid to take the organisation into a new age, moving from its grassroots base to a having an overseeing board.
It was a tumultuous time and there was a lot of fallout over the Kennett government decision to merge the Fairfield Hospital, which treated HIV-positive people, with the Alfred and Royal Melbourne hospitals.
Current VAC president Kevin Guiney said it was vital community organisations continued to work in HIV prevention as the message could be easily lost.
-œThe health minister during the [early ’90s] was Marie Tehan and she wanted to put a stop to a lot of the things the VAC was doing -” she didn’t think we were doing the right thing, he said.
-œI think there was an old campaign of two boys kissing … which she tried to stop and we funded it ourselves and she got very upset that we did. It was a turning point from the point of view that if we couldn’t get the money from the government to do it, we’d raise it in the community. We’re not aiming at bureaucrats, we’re aiming at people on the street and in the community.
While other states have maintained steady HIV rates over the years, the number of HIV infections in Victoria started to climb from 2000.
The VAC/GMHC says with HIV and STI prevention back on the agenda and, more importantly, in the last state budget, the issue of HIV has again become a priority.
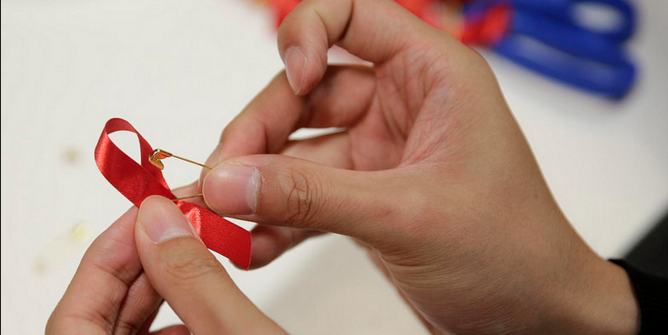
But while the VAC continues to battle it out in the scramble for government funding, there is one thing it can always rely on Â-” its army of voluteers that has been its constant saviour.